 Parents: Holly and Mike
Parents: Holly and Mike
Hometown: Des Moines, Iowa
Born July 14, 1997
Morgan’s Story
“When Morgan was born I often said, ‘Morgan doesn’t deserve this.’ Mike always said, ‘deserves got nothing to do with it.’ It’s true, things happen whether we really deserve them or not, and it’s not just bad things, but good things, too. All things being equal, all things are not equal. It is hard for us to really tell what is fair or not. We just trust that God knows what He is doing and make the best of the situation that is handed us.”
And make the best of the situation they have. When Holly was in the early weeks of her first pregnancy, Mike was advised that he might be a carrier for a balanced translocation between chromosomes 9 & 18, as his niece had a partial trisomy caused by an unbalanced translocation. Mike had the blood test and found that he was indeed a carrier. They decided then at 18 weeks gestation to have the amniocentesis to find out if their baby was indeed affected. Holly remembers getting the results from the amnio over the phone and learning that their baby had an unbalanced translocation resulting in a partial trisomy of the long arm of chromosome 18 and partial monosomy of the short arm of chromosome 9. “For us, we believed that this child only had one chance to survive and that was to carry him to term. That made our decision pretty easy our baby wouldn’t have a chance if he was never born.“ The news was passed on to family and close friends soon after receiving the results of the amnio. Holly told her supervisors at work a few months later and by the time she was in her sixth month a few of her co-workers knew that there was a problem, but she never went into specifics with those outside the family.
 When asked how they have made it through the challenges of carrying to term, Holly replies, “God gave us this child for a reason and He had given our child trisomy 18 for a reason. It didn’t matter that we didn’t understand why this happened, it only mattered that we trusted that there was a reason for this happening. Knowing the reason why would not change anything.
When asked how they have made it through the challenges of carrying to term, Holly replies, “God gave us this child for a reason and He had given our child trisomy 18 for a reason. It didn’t matter that we didn’t understand why this happened, it only mattered that we trusted that there was a reason for this happening. Knowing the reason why would not change anything.
“During my pregnancy I think I felt more alone in the world than I ever have. Of course, the wonderful Trisomy 18 website did not exist then. It wouldn’t have mattered anyway; we did not have a computer. We knew nothing about t18 except what the doctors told us. Even though Mike was diagnosed as a balanced translocation carrier we were not referred to a genetics counselor or a geneticist. We knew of one other child living with Trisomy 18 Morgan’s cousin she was 6 months old at the time of Morgan’s diagnosis.
“I never want anyone to have to feel that loneliness, that feeling of being different from everyone else. Even in a crowd of people you know you aren’t like anyone else, your baby isn’t like anyone else’s baby. Our families were supportive, but not exactly understanding of the situation. They felt like as long as the pregnancy went fine the baby would be fine. It was hard emotionally to have to try to explain this over and over again. Mike and I really tried to keep it all together, after all, we had to take every piece of information we received and decide whether we would take it as the ‘gospel truth,’ or whether we should be cautiously optimistic.
“Mike was a lifeline for me, at this time. Every time I felt sad or cried he would tell me I had to keep a positive attitude, it wasn’t good for the baby or for me to be too depressed or sad. Plus, he constantly reminded me that we did not know for sure what would happen. We would wait and see. For me, the not knowing, while being excruciatingly difficult, was better than a barrage of bad news. I could handle the, ‘We just don’t know what will happen,’ ‘We will have to wait and see,’ ‘We don’t have an answer for that’ much better than hearing that the doctors 100% expected our baby not to live.”
Holly’s blood pressure was high during her third trimester, so the decision was made to induce her three weeks early. She went into the hospital early on the morning of Monday July 14th. They broke her water and started oxytocin. After just over four hours Holly started bleeding quite badly. Doctors, unsure of where the blood was coming from, quickly extracted Morgan via forceps. While the neonatal team took him to the warmer to check him over, Holly’s doctor confirmed that her placenta had abrupted, which was what had caused the bleeding.
Once her placenta had been dealt with, Holly was given five short minutes to hold Morgan. She remembers her first impressions, “He was so beautiful already the spitting image of his daddy! And he had a full head of dark hair!”
Mike went with Morgan to the NICU, as they had decided prior to Morgan’s birth. Holly had insisted that Mike was to go with him and not worry about her that he was to stay with Morgan as long as possible to find out as much information as he could about Morgan’s condition. Holly was finally able to get down to the NICU around 3pm, and was allowed to hold him. “When they first asked if I wanted to hold him, I said, ‘no’. I didn’t want to take him out of his warm bed and hold him if it would upset anything they were doing with him. The nurses insisted that I take him and it was love at second sight.”
Later that afternoon, back in Holly’s room, the doctor and a social worker came to visit Holly and Mike. They took out a list of about 20 different things that were ‘wrong’ with Morgan most were trivial: an anterior hair whorl, fingerprints whorled, his 2nd and 3rd toes joined together (called syndactyly), short toenails, short tapered fingers, etc. The main thing they told them was that they did not expect Morgan to survive to the end of the week. Holly refused to accept this. She sat and listened and nodded, but thought Mike was crazy when he broke down in tears. “I just knew it wasn’t going to happen.” All the same, the family priest came and baptized Morgan at the hospital the next day.
 Morgan was born with esophageal atresia and a tracheo-esophageal fistula, and after several days Mike and Holly were given a couple of different surgical options as to how they could deal with this. “Morgan seemed in relatively good health he had no heart problems, no respiratory problems, nothing that should necessarily make surgery difficult so we decided we would do whatever it took to help him have as normal a life as he could. That meant making decisions as they arose and then never second guessing ourselves after a decision had been made. Many times we asked ourselves, ‘Does the fact that Morgan has t18 have any relevance to this decision? What would we do for him if he was any other child?’ When it has come to making decisions regarding improving his life, we have always been very aggressive. We give him the opportunity for growth and development and what he accomplishes is his own reward.”
Morgan was born with esophageal atresia and a tracheo-esophageal fistula, and after several days Mike and Holly were given a couple of different surgical options as to how they could deal with this. “Morgan seemed in relatively good health he had no heart problems, no respiratory problems, nothing that should necessarily make surgery difficult so we decided we would do whatever it took to help him have as normal a life as he could. That meant making decisions as they arose and then never second guessing ourselves after a decision had been made. Many times we asked ourselves, ‘Does the fact that Morgan has t18 have any relevance to this decision? What would we do for him if he was any other child?’ When it has come to making decisions regarding improving his life, we have always been very aggressive. We give him the opportunity for growth and development and what he accomplishes is his own reward.”
The surgery, performed at 10 days of age, was successful. While under anesthetic, doctor’s also placed a g-tube so that Morgan could be fed directly into his stomach. Unfortunately after his esophagus surgery he developed a chylothorax, or a hole in the thoracic duct. It is a known, but not common, complication of chest surgery. It is caused by a doctor nicking the duct.
That morning they got a phone call from the hospital at 5 am. They wanted Mike and Holly to come to the NICU early that morning, as quickly as they could get there. When they asked what the problem was, they were told that Morgan had had many, many apnea episodes throughout the night and they thought he couldn’t keep on like this. They wanted them to come to see him right away. After hanging up the phone Holly cried out to Mike, “Why now? Why is this happening now?! They told us he might be coming home in another week. He was getting better.” (At this point they didn’t really know the nature of Trisomy 18 yet.) “Mike, it’s not supposed to be this way. We are supposed to be a family, we are supposed to be together!”
Holly recalls this as her darkest moment. “I told Mike, ‘He will leave us and he will be all alone.’ ‘He won’t be alone,’ Mike snapped at me. I realized what I had said. ‘Of course, he won’t be alone. Your mom and dad raised five boys; they will know how to take care of him for us. They will be waiting for him.’”
When they arrived at the hospital, the neonatalogist told them that it was the beginning of the end for Morgan. Morgan was due to have a chest x-ray that day to check on the surgical site and they decided to go ahead with it in spite of these spells. Holly will be forever grateful to the radiologist, as he discovered that the source of Morgan’s apnea spells was a chest cavity full of fluid.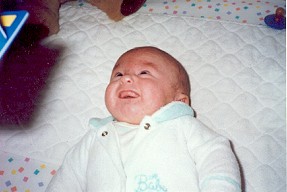
Once the fluid was identified, doctors then had to determine what was causing the fluid to build up. To do this, the doctor had to extract the fluid from Morgan’s chest. After analyzing it, it was found to be chyl, the contents of the thoracic duct. Mike and Holly were told there was nothing they could do to repair it, it had to heal on its own. It was usually a six week or longer process and Morgan would have to stay in the hospital during this time. Doctors also explained that the best way for the hole to close was to let the pressure build up in Morgan’s chest to hold the hole closed. That meant letting Morgan go with fluid in his chest for as long as he could keep his SATS up. The more often they had to drain his chest the more fluid that would come out of the thoracic duct and re-accumulate.
“We had to watch our little boy gasp for air one night. Finally, I couldn’t take it anymore and asked for the doctor to come. She came and extracted 120ccs from his chest. She told us that every time they put the needle into his chest they were risking a pneumothorax (hole in the lung) and that if the fluid built up again they would put in a chest tube. She told us that a chest tube is quite painful and they had hoped to not have to do it. Well, she told us this with Morgan listening. I guess he decided that didn’t sound good to him because after that there was no more fluid build up. In fact, the doctor told us she had never seen a chylothorax heal that quickly.”
By the time Morgan was six weeks old, he was ready to come home. Holly recalls, “When Morgan came home, at six weeks old, we had no help. There was no nursing set up for us; there was no hospice, just Mike and me. Talk about feeling all alone. We had gone from 24-hour-a-day intensive care nursing to us taking care of our baby at home. As we drove home I felt the weight of it all on my shoulders. I was terrified something would happen.”
“For nearly a month I was nauseous most of the time, but especially when I had to leave Morgan (with his dad) to get groceries or whatever. I literally was near throwing up all the time. Morgan had an apnea monitor at home, not because the hospital wanted us to have it, but because I had insisted. I couldn’t survive without it! Not once in six months did he have an apnea episode and finally the insurance company said they wouldn’t pay for it anymore. Luckily, by then I was a bit more relaxed.“
 When Morgan was nine months old Holly and Mike saw a geneticist and genetic counselor from the University of Iowa. That was their first meeting with any one in the field of genetics! Holly writes, “I had already determined that my main question for them was going to be, ‘what is going to make Morgan die?’ He seemed so healthy to me, but most doctors still did not expect him to survive. We had gone through the appointment, the doctor examined Morgan, and we sat at a table talking. They were so kind to us that I had forgotten my question.”
When Morgan was nine months old Holly and Mike saw a geneticist and genetic counselor from the University of Iowa. That was their first meeting with any one in the field of genetics! Holly writes, “I had already determined that my main question for them was going to be, ‘what is going to make Morgan die?’ He seemed so healthy to me, but most doctors still did not expect him to survive. We had gone through the appointment, the doctor examined Morgan, and we sat at a table talking. They were so kind to us that I had forgotten my question.”
“The doctor got up to leave and he said he thought he would see us back in a year or 18 months. I looked at him and said, ‘You mean you expect Morgan to still be alive in another year?!’ The doctor looked at me like I was crazy, but said he did expect things would continue as they were. I told him he was the only one. ‘What do you mean?’ he asked. I explained some of the attitudes I was getting. He came back into the room, sat down and proceeded to tell us that because Morgan was in general good health had no heart, respiratory, kidney problems, nothing that was life threatening he didn’t feel that Morgan was going anywhere for awhile. The weight was lifted in that moment. Our lives were never going to be the same again. We didn’t have to feel a constant worry or dread; we could enjoy everything without living for the moment all the time. We could actually plan ahead. We could plan for Morgan’s first birthday.”
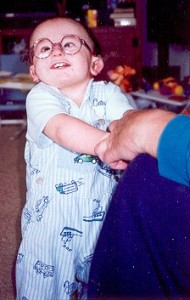
Since that time Morgan has thrived, and has often baffled his doctors by failing to follow the “rule book”. One example of this that was very confusing for everyone involved was Morgan’s hearing. Morgan had a hearing test administered in the NICU before he was discharged, which he failed. For this reason, he was scheduled for a follow-up appointment at five months of age. The tests were done and the results came back that Morgan had a moderate to severe hearing loss. The audiologist did, however, feel that Morgan had enough hearing to warrant using hearing aids for Morgan.
Morgan was fitted with hearing aids soon after, but they never did work properly. They produced constant feedback, and Morgan’s ear canals were so tiny that they couldn’t get a good fit for the hearing aids with the ear molds. Holly took Morgan in repeatedly to achieve a successful fit and find an end to the feedback. All the same, the effort seemed worth it Morgan started vocalizing after just one month of wearing the aids.
The feedback issues never did resolve themselves, however, and by the time Morgan was three and starting preschool, he had begun pulling the hearing aids out, crying when Holly tried to put them in for him, and even swallowing a piece of one of the aids one night. Unable to find any cause for this change of behaviour, Holly took Morgan to participate in a new hearing test at the University of Iowa. It was then and there that Holly found out the reason for Morgan’s behaviour his hearing was completely normal! No one really knows how this could be whether the first test was incorrect, whether Morgan’s audio development was simply delayed due to his Trisomy 18 but it is simply one example of the many times that Morgan has “re-written” the rules for himself!
“In the years following Morgan’s first year things haven’t been so challenging, at least in the sense of fighting attitudes against him. As he has grown up everyone realizes that they have to consider him as they consider any other child. His doctors are now some of his biggest cheerleaders. Most of the obstacles we have faced have been of our own making and they seem to be more mine than Mike’s. One of the biggest fears we have now is actually of Morgan out surviving us. If he lives longer than we do, what will become of him?! We can provide for him, setting up a trust, lining things up now, but who will be there for him, who will love him like we do?! It is a terrible dilemma, as a parent, to think that maybe you don’t want your child to live longer than you do.”
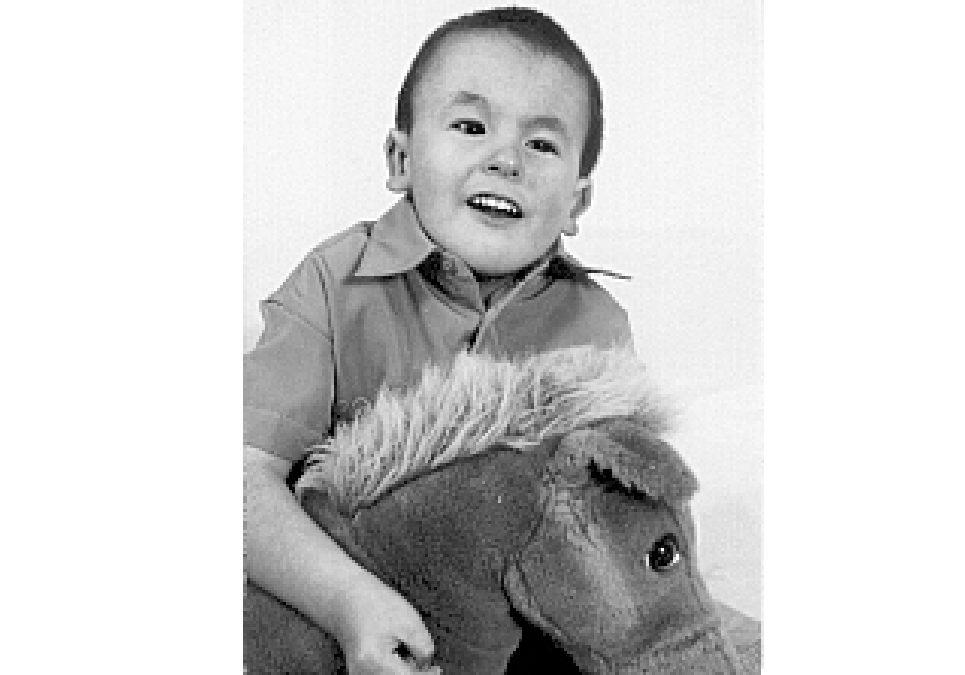
In the beginning a physical therapist, occupational therapist, special education teacher, and a teacher for the hearing impaired came for therapy at their home through the Early Childhood Intervention Program. At age three, Morgan started the preschool program, attending school four days a week for three hours a day. There were all the standard fun activities for preschool the most important being play, friends and swimming! – but Morgan’s time at school included therapy as well. At three, Morgan also started at the local Children’s Hospital therapy programs. At physical therapy Morgan learned how to sit independently, to stand and to take steps both independently and with a gait trainer called a Pacer. He also participated in occupational therapy bouncing for stimulus, using his hands to choose toys, and learning how to eat by mouth and eventually how to feed himself. Perhaps one of his most prized therapies, however, is horseback riding!
 His horseback riding has had a profound impact on both Morgan’s development as well as his physical condition. In May 2002, a yearly x-ray showed that Morgan had a 19 degree curve of his spine. The doctor wasn’t concerned, stating that it wasn’t serious and there was nothing they would do for a curve that slight, but that she did need to watch it, and if it started to progress then we would have to consider some bracing. In June of the same year Morgan started a therapeutic horseback riding program. He went weekly all summer, fall and up until Christmas. Of course, he loved it! One of the big changes Holly and Mike saw was that after only three months of riding Morgan started sitting on the floor without using his hands to help. He would pick up his hands and play with objects while sitting. Morgan’s physiotherapist attributed much of that to his riding. His trunk control just continued to get better and better. In May 2003 Morgan had a new x-ray of his back. The doctor came in and said he had no scoliosis. She was really surprised. She felt perhaps some of the curve in the previous x-ray could have been positional, but really said she had rarely seen scoliosis get better. You can stop the curve from progressing, but it doesn’t generally go away. She thought the horseback riding played a big part in this.
His horseback riding has had a profound impact on both Morgan’s development as well as his physical condition. In May 2002, a yearly x-ray showed that Morgan had a 19 degree curve of his spine. The doctor wasn’t concerned, stating that it wasn’t serious and there was nothing they would do for a curve that slight, but that she did need to watch it, and if it started to progress then we would have to consider some bracing. In June of the same year Morgan started a therapeutic horseback riding program. He went weekly all summer, fall and up until Christmas. Of course, he loved it! One of the big changes Holly and Mike saw was that after only three months of riding Morgan started sitting on the floor without using his hands to help. He would pick up his hands and play with objects while sitting. Morgan’s physiotherapist attributed much of that to his riding. His trunk control just continued to get better and better. In May 2003 Morgan had a new x-ray of his back. The doctor came in and said he had no scoliosis. She was really surprised. She felt perhaps some of the curve in the previous x-ray could have been positional, but really said she had rarely seen scoliosis get better. You can stop the curve from progressing, but it doesn’t generally go away. She thought the horseback riding played a big part in this.
Recently Morgan seemed to have developed what Holly and Mike thought might be seizures. He saw a neurologist in August of 2003 and Morgan had an EEG and an MRI done at that time. Holly remembers that “during the EEG the technician started asking me questions like, ‘Has he had an EEG before?,’ and ‘He isn’t on any medication now?!?’ and ‘Do you have an appointment to see the doctor today?’ I asked her what the problem was, since I knew with questions like that she had to be seeing something. She said she really couldn’t say much, but that we should call our pediatrician if we didn’t here from them by the end of the day.”
They saw the neurologist again a week later and found out at that time that Morgan’s EEG was very abnormal that he seemed to be having generalized seizures. They described again for the doctors what the seizures looked like, and were told that Morgan had developed Infantile Spasms a rare seizure that mostly occurs in children under two years of age. These seizures can unfortunately be very hard to control, and can evolve into another type of seizure if left uncontrolled. More frightening still for Holly was the fact that children who have this condition tend to regress mentally and lose skills often never getting them back. Despite the fact that this condition is almost unheard of in older children, the neurologist feels that it has occurred at this age because of the fact that Morgan’s brain is maturing slower than normal due to his Trisomy 18.
Since the diagnosis Holly has had two good pieces of news: the first is that Morgan hasn’t lost any of his skills or regressed at all which is particularly encouraging since it has taken him so much work to gain those skills in the first place. The second is that as of November 8th when a second medication was added to his initial seizure medication, Morgan has been seizure-free.
 Although Morgan has lived a lifetime of special memories, the whole family was absolutely thrilled when Morgan was granted a wish from the Make a Wish Foundation. In December of 2003 the family traveled down to Walt Disney World for a whirlwind week of excitement and special memories. As always, Morgan was a star!
Although Morgan has lived a lifetime of special memories, the whole family was absolutely thrilled when Morgan was granted a wish from the Make a Wish Foundation. In December of 2003 the family traveled down to Walt Disney World for a whirlwind week of excitement and special memories. As always, Morgan was a star!
The road has not always been simple, but Holly is quick to point out that she doesn’t do anything that every other mother on earth does she simply loves her son. “The refrain from a song by Garth Brooks probably says it all. ‘It was your song that made me sing. It was your voice that gave me wings. It was your light that shined guiding my heart to find this place where I belong. It was your song.’
The book “Expect a Miracle” by Dan Wakefield was something Holly first listened to on tape during her pregnancy twice! “At first it gave me a feeling of urgency, like I needed to hurry up and do something to save my baby. It made me feel like somehow I could heal my child. The second time through the realization hit me that my baby would be the miracle, even if he wasn’t cured. Maybe the changes he made in my life would be the miracle.”
“I hear from people sometimes about what a wonderful job we do with Morgan. He is lucky to have us as parents etc., etc., etc. I don’t really take much credit for what Morgan has accomplished. We have given him the opportunity, but he does all the work. If he doesn’t want to do something I certainly can’t make him! He has to decide whether it is worth his effort to do certain things. Sometimes I wish I could make him do some of the things I want him to, but that’s not happening. Recently, I decided maybe Mike and I should take some of the credit for Morgan’s growth. After all, we brought home this tiny, fragile baby that was g-tube fed and WE DIDN’T KILL HIM!!! He actually survived us to be 6 1/2 yrs. Old!”
“I am thankful for Morgan’s continued good health. Also, for my best friend, Shawna, who has always meant the world to me, and has stood by us through Morgan’s entire life. She is a blessing in Morgan’s life today as much as in mine and Mike’s. I am also thankful for a wonderful priest, Father Mike, who told us, ‘Some people believe that God answers all prayers, but sometimes the answer is no. I believe that God answers all prayers, sometimes the answer is ‘not now.’
“I hear so much hopelessness in regards to t18 and it just breaks my heart. I think that one has to continue to have hope for their child because sometimes that is all there is just hope. Sometimes that is enough to get you through the hard time, especially when the diagnosis is so new. Everyone hopes for something different and that is okay just don’t lose hope. Hope for the best possible outcome for your baby, hope that your baby will be born alive and you will be able to spend some time with it, hope that you can continue to enjoy the baby’s movements within the womb, whatever it is, hold onto it.”
